TBI-related Emergency Department Visits, Hospitalizations, and Deaths (EDHDs). (2019, March 29). Retrieved from https://www.cdc.gov/traumaticbraininjury/data/tbi-edhd.html
Traumatic Brain Injury Information Page. (n.d.). Retrieved from https://www.ninds.nih.gov/Disorders/All-Disorders/Traumatic-Brain-Injury-Information-Page
Pearl. (2017, February 17). Brain Injuries due to Motorcycle Accidents. Retrieved from https://chicagoinjurycenter.com/motorcycle-accident-brain-injuries
Athletes and TBI: Sports-Related Traumatic Brain Injury (TBI) (n.d.). Retrieved from https://braininjuryeducation.org/Populations/Athletes/
L. R. (2021, March 16). Russian hockey player Timur Faizutdinov dies at 19 after being hit in the head by a puck. Retrieved from https://www.msn.com/en-us/sports/nhl/russian-hockey-player-timur-faizutdinov-dies-at-19-after-being-hit-in-the-head-by-a-puck/ar-BB1eE0QY
Suicide Prevention: D’Amore. (2020 November 21). https://damorementalhealth.com/orange-county-mental-health-treatment/suicide-prevention/
Thys, F. (2019, March 11). ‘What Does War Do To An Entire Person?’ – VA Studies Veterans With Blast Injuries. Retrieved from https://www.npr.org/2019/03/11/702196238/what-does-war-do-to-an-entire-person-va-studies-veterans-with-blast-injuries
Trotter, B. B., Robinson, M. E., Milberg, W. P., McGlinchey, R. E., & Salat, D. H. (2015). Military blast exposure, ageing and white matter integrity. Brain : a journal of neurology, 138(Pt 8), 2278–2292. https://doi.org/10.1093/brain/awv139
Traumatic Brain Injury and PTSD: Focus on Veterans (2018, September 02). U.S. Department of Veterans Retrieved from https://www.ptsd.va.gov/professional/treat/cooccurring/tbi_ptsd_vets.asp
PTSD and Trauma Treatment in Orange County: D’Amore. (2020, October 15). Retrieved from https://damorementalhealth.com/orange-county-mental-health-treatment/trauma-ptsd/
Tony, Kristy PT, DT. (2018 April 10) TBI and the Non-Athlete Population. https://braininjurymn.org/annual_conference/CONF-2018-presentations/Fri-I-D.pdf
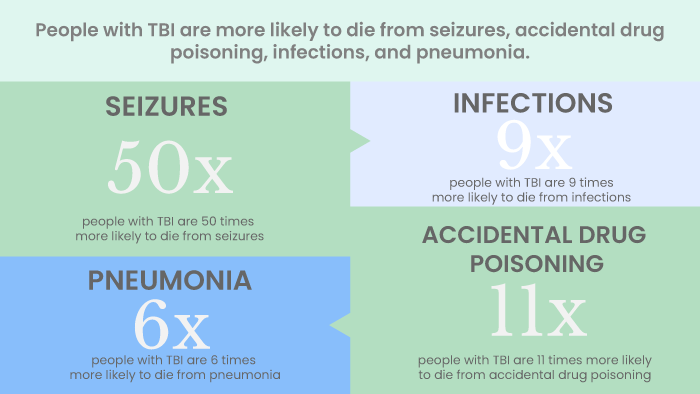
CDC. Moderate to Severe Traumatic Brain Injury is a Lifelong Condition. https://www.cdc.gov/traumaticbraininjury/pdf/moderate_to_severe_tbi_lifelong-a.pdf
Bullock, G. (n.d.). (2019 March 18) Long Term Effects of Moderate or Severe Traumatic Brain Injuries (TBI). Retrieved from https://www.theraspecs.com/blog/long-term-effects-of-moderate-severe-traumatic-brain-injuries-tbi/
TBI Treatment in Orange County, CA: D’Amore. (2020, October 09). Retrieved from https://damorementalhealth.com/traumatic-brain-injury-treatment/
Equine Therapy for Mental Health. (2020, October 16). Retrieved from https://damorementalhealth.com/equine-therapy/
Experiential Therapy. (2020, December 07). Retrieved from https://damorementalhealth.com/experiential-therapy/