Veterans returning home from World War I who suffered from significant and long-lasting emotional and physiological distress as a result of their experiences were said to be “shell-shocked.” After World War II, it was called “combat fatigue.” We now refer to the range of symptoms that may occur due to deep trauma as “Post-Traumatic Stress Disorder” or “PTSD.”
PTSD is a specific clinical diagnosis that results from experiencing severe trauma or a life-threatening event. People who have served in the military have almost twice the risk of developing PTSD than the average population. 1
It is normal and natural for the mind and body to react with shock after something extremely traumatic or life-threatening occurs. Still, when that reaction persists long after the event has passed, PTSD may or may have already developed.
The prevalence of PTSD varies widely across different wars and eras. The rates of PTSD amongst those who fought in Iraq and Afghanistan are thought to be as high as 20-30%. At least 500,000 U.S. soldiers who served in these wars have developed PTSD.
Urban-style warfare may be a factor in this; guerilla attacks, roadside explosives, and confusion between battle zones and safe zones may trigger more cases of PTSD than “conventional fighting”.
On top of this, survivability has greatly increased. Protective gear and battlefield injury support have improved enormously, meaning veterans are surviving horrific life-threatening injuries that they wouldn’t have survived before. And they are returning home with physical injuries on top of the psychological trauma.
Comorbidity (simultaneous medical conditions) is also higher in PTSD in veterans than in the general population.
Veterans with comorbid PTSD and AUD (as well as other types of drug abuse) are more difficult to treat as a result of poor social functioning, more suicide attempts, and less adherence to treatment. 5
There are 4 categories of symptoms that define PTSD: Re-experiencing symptoms, avoidance symptoms, arousal, reactivity symptoms, and cognition and mood symptoms. To receive a PTSD diagnosis, one must experience at least one symptom from each category for at least one month. 2
Re-experiencing symptoms are likely to cause problems in your everyday routine. They can be in the form of flashbacks, bad dreams, or frightening thoughts.
It’s normal to experience nightmares after a serious car wreck or have frightening thoughts after your house has been broken into. For someone experiencing PTSD, however, those feelings can be debilitating. The nervous system gets stuck in a loop, and your brain is telling you that you are still in just as much danger as you were when the event occurred.
These aren’t just bad dreams that you can shake off as your day goes on. These nightmares and flashbacks take your mind and body right back to where you were when the trauma occurred.
Emotional avoidance is when you avoid thoughts or feelings about the traumatic event you experienced.
Behavioral avoidance is when you avoid situations and other external factors that remind you of the traumatic experience.
Someone who is emotionally avoidant may try to remain distant from any unpleasant emotion, such as fear or anger. They can do this by shutting down emotionally, drinking alcohol, or taking drugs to numb out or not feel anything.
Behavioral avoidance is more visible to the outsider. A behaviorally avoidant veteran may stop watching the news or scrolling through social media to avoid any stories about current military events. They may avoid crowded places, fireworks shows, or sweltering weather, depending on what reminds them of the traumatic event.
Arousal and reactivity symptoms can look like hypervigilance or an exceptionally sensitive startle reflex. Common everyday noises, like a car door slamming, can make you jump out of your skin; convince you that you are in immediate danger.
Hypervigilance can make it difficult to concentrate or sleep. This can lead to feelings of frustration and anger, which can worsen the symptoms of PTSD even further. Feeling jumpy and ill-at-ease all the time is exhausting and can be very disheartening and depressing.
Many people with high levels of reactivity symptoms turn to alcohol and other drugs in order to numb their senses and feel less reactive to the world around them.
Cognition and mood symptoms may present in the form of depression or loss of interest in enjoyable activities. You may have persistent negative thoughts about the world, or yourself. You may feel irrational guilt or blame for the event, or even things currently going wrong in your everyday life that have nothing to do with the traumatic event.
Cognition and mood symptoms may begin right after the event, or months or even years later. These types of symptoms are not the result of drug and alcohol use, or a brain injury. These symptoms can make you feel detached from your loved ones, and the world around you.
Any and all of these symptoms are completely normal for a few weeks after a traumatic event. PTSD means that you’ve been experiencing at least one symptom from each of these 4 categories for a month or more, and they are interfering with your ability to live your life.
PTSD makes everyday life challenging, even unbearable for a prolonged period of time. PTSD is often accompanied by depression, substance abuse, or other anxiety disorders. 2
There are 3 main factors that determine whether or not a particular event will lead to the onset of PTSD after the trauma has occurred:
Saliency refers to how “bad” the event was. The louder, harsher, more violent the event is, the more likely PTSD will result.
Genetics for the individual is all about luck, or lack of luck. Twin studies are an excellent example of this. One twin can go off to war and come back shaken but emotionally sound, while the other will go and experience all of the same things and come back with PTSD. You don’t know how your genetic makeup will affect your reaction to specific circumstances.
If someone has experienced trauma in the past, it is more likely that future trauma will bring about the onset of PTSD. The brain and the nervous system can only handle so much. 3
For veterans, the likelihood of PTSD occurring after deployment depends on these factors:
The factors that determine the likelihood of PTSD occurring are incredibly individualized to each person. No two cases are the same, and there is no way to accurately determine whether or not someone will develop PTSD in the future.
It does help to understand what may contribute to PTSD and recognize the symptoms of PTSD when they occur.
PTSD is one of the most common disabilities for veterans of the Iraq and Afghanistan wars. 4 When PTSD goes untreated, the likelihood of other symptoms developing increases.
PTSD isn’t likely to resolve on its own. The longer it goes untreated, the more likely those resulting symptoms will further decrease the quality of life for the individual suffering (as well as for their family and loved ones).
The symptoms that may result from untreated PTSD aren’t limited to emotional and psychological; physical maladies can also occur.
Some of these conditions are life-threatening and include:
Suicide is also a risk for untreated PTSD, especially if depression, anxiety, and substance abuse disorders become a problem.
If you or someone you love lives with PTSD and you’re not receiving treatment, reach out for help sooner rather than later. If you believe you or the person you love may have undiagnosed PTSD, call your doctor or a professional therapist as soon as possible. There is a treatment for PTSD, and the suffering doesn’t need to get worse before it gets better.
Veterans who return home from combat are prone to PTSD that occurs with repeated trauma over a prolonged period of time. This type of PTSD can be more difficult to treat, which is why it’s so important to get help as soon as possible after becoming aware of your symptoms or being diagnosed.
Trauma-focused psychotherapy is highly recommended for veterans who have been exposed to repeated life-threatening and horrific events. This involves focusing on the trauma and working through the difficult memories using various techniques with the guidance of a therapist. 4
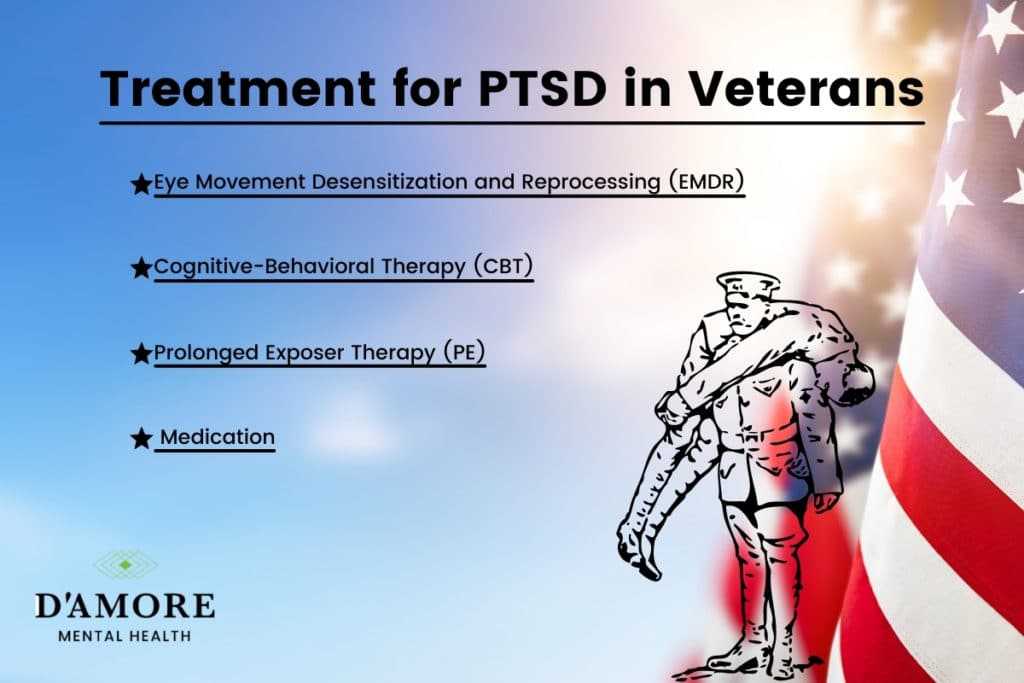
Cognitive-behavioral therapy (CBT) focuses on identifying, understanding, and changing your thinking and behavioral patterns. This is an active type of therapy, where the patient learns and utilizes specific skills for dealing with PTSD symptoms in everyday life. 6
Prolonged exposure therapy (PE) is conducted with the belief that symptoms of PTSD are the result of cognitive and behavioral avoidance of anything trauma-related. PE therapy works to reverse that avoidance with corrective information and the organization and processing of the memories associated with the trauma. 7
Eye movement desensitization and reprocessing (EMDR) focus on a back-and-forth movement or sound while recalling the trauma to understand better and process what you went through. The premise is that people with PTSD are confused and unclear about the trauma, and this technique clarifies the event so that you can understand it better, and therefore recover from it. 8
Medication, specifically selective serotonin reuptake inhibitors (SSRIs), can effectively regulate emotions in PTSD patients. They are a class of medication used for treating depression and anxiety and have been approved by the FDA specifically to treat PTSD. 9
Some people are unable to focus on or commit to therapy until their moods have leveled out. Using medication in combination with therapy can be life-changing for those who have mood disorders due to their PTSD.
Recovery from trauma is an ongoing process, and it’s important to understand that the trauma has occurred; it will never be undone. Moving forward entails learning to live with what has happened – not undoing it, not pushing it away, not forgetting about it. Denying the experience, or trying to bury it will only increase and prolong your suffering in the long run.
The mind-body connection is fascinating, and professionals are (thankfully) beginning to embrace the idea that they’re connected. We’re stepping away from treating just individual symptoms, and stepping towards treating the whole person; mind, body, and soul.
The people you hang out with have a bearing on your emotional state – as do the books you read, the TV you watch, and the news cycle you follow.
What you eat, how you sleep, and the information that you take in each day has an effect on your cognitive functioning and emotional responses. Choose wisely. No one is saying everything you read and watch needs to be happy and upbeat, but on the other hand, it’s also not necessary to feed your depression and anxiety by focusing on the dark aspects of entertainment or human nature.
Drinking alcohol or smoking marijuana can be very tempting when you feel overwhelmed with depression and anxiety, especially if you’re living with PTSD. The use of substances might bring about temporary relief, but in the long run you risk falling into dependence or addiction – which will just make your recovery that much more difficult and complicated.
PTSD is a diagnosable condition that requires professional treatment. Never try and treat yourself, or forgo treatment for something so serious.
There are things you can focus on in your everyday life to make treating your PTSD a little less painful; make your life more bearable and healthier for yourself and the people who care about you.
Nature is healing and uplifting, and so are endorphins. Being outside in the fresh air and sunshine can do wonders for the mood. Add in some hiking, running, kayaking, or kite-flying, and you have a recipe for endorphins and contentment. This won’t cure your PTSD by any means, but it may help you sleep better, increase your appetite, and perhaps even remind you that the world is a beautiful place – even for just a few hours at a time.
Yoga and meditation are becoming more mainstream by the day. There’s a reason for this – it helps you to remain in the present moment. Memories cause PTSD from the past. Paying attention to your breath or maintaining a difficult pose keeps you grounded in the present, where you are safe.
Essential oil diffusers are another increasingly popular home addition. Certain smells can be mood-enhancing, energizing, or soothing. If the smell of baking cookies gives you pleasure, buy some vanilla-scented oils. You can even place some on your pulse points and carry it with you throughout your day.
Isolation is tempting when dealing with any psychological ailment, whether it’s depression, anxiety, addiction, or PTSD (or all 4). It may be challenging, but pick up the phone when you can. Meet up with other Vets for coffee, take your nephew to a movie, make a dinner date with a trusted friend. You don’t need to discuss your PTSD, but being around other people can be refreshing; it can get you out of your head for just a little while.
Post-traumatic stress disorder is complicated and overwhelming. It requires treatment and attention. However, it does not have to define you, and you don’t have to suffer for the rest of your life. More and more research and understanding of PTSD comes out every day, and the stigma of mental health issues is fading rapidly.
If you or someone you care for has PTSD or you suspect that they may have PTSD, don’t wait to ask for help. The sooner you start addressing the trauma you survived, the sooner you can begin to thrive again. There is help, there is hope, and there is recovery.
1. PTSD and Veterans: Breaking Down the Statistics. (2021, May 11). Retrieved from https://www.hillandponton.com/veterans-statistics/ptsd/
2. Post-Traumatic Stress Disorder. (n.d.). Retrieved from https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/
3. Rick Doblin: Overcome Trauma. MDMA, PTSD & Healing. (n.d.). Retrieved from https://www.bialikbreakdown.com/watch-podcast/ability-to-heal
4. What Happens If PTSD Goes Untreated?: DisabledVets. (2021, June 23). Retrieved from https://www.disabledvets.com/faqs/what-happens-if-ptsd-goes-untreated/
5. Reisman, M. (2016, October). PTSD Treatment for Veterans: What’s Working, What’s New, and What’s Next. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5047000/
6. PTSD Facts & Treatment: Anxiety and Depression Association of America, ADAA. (n.d.). Retrieved from https://adaa.org/understanding-anxiety/posttraumatic-stress-disorder-ptsd/treatment-facts
7. Prolonged Exposure Therapy for PTSD (PE). (n.d.). Retrieved from https://deploymentpsych.org/treatments/prolonged-exposure-therapy-ptsd-pe
8. VA.gov: Veterans Affairs. (2018, August 10). Retrieved from https://www.ptsd.va.gov/understand_tx/emdr.asp
9. JR; H. R. (n.d.). Selective serotonin reuptake inhibitors in post-traumatic stress disorder. Retrieved from https://pubmed.ncbi.nlm.nih.gov/10757257/